WHO officials said that they are trying to expedite delivery of mpox vaccines to outbreak-stricken DR Congo through talks with the world’s only two mpox vaccine manufacturers, as well as appeals for vaccine donations and negotiations with DRC officials.
But speaking at a press briefing on Thursday, WHO’s Dr Mike Ryan, Executive Director of Health Emergencies, and technical lead Maria Van Kerkhove were unable to provide concrete details as to when significant quantities of vaccines could be rolled out – and how many, in light of the global shortage of supplies.
Despite two years of millions of doses of global mpox vaccine rollout, there has been no mass administration of the vaccines so far in DRC or other west African countries. This is despite the fact that the region, and DRC in particular, is now the epicenter of the largest and deadliest mpox outbreak to date.
The problems are multiple – ranging from global supply lines to local regulatory hurdles, stigma around mpox and vaccine hesitancy.
At the global level, the production line of Bavarian Nordic, the Belgium-based manufacturer of one the world’s two available mpox vaccines, MVA-BN, halted its production for months in 2022 due to building renovations.
Then in August, 2023, it received a $120 million contract from the US Biomedical Advanced Research and Development Authority (BARDA) to manufacture new mpox vaccine product in bulk. But that has only partly restored the depleted US stockpile – believed to be the world’s largest.
At the same time, stigma around the disease, which can be sexually transmitted, as well as around vaccines more generally has also held back progress in the DRC – one of the most vaccine-hesitant countries in Africa.
An attempt to donate doses of mpox vaccine was stalled for more than a year, Bavarian Nordic Chief Executive Paul Chaplin said in a statement to Reuters, in December 2023. National regulatory approval of vaccines and medicines has thus inched forward at snail’s pace.
Taking gloves off to join in partnership

“We know that production capacity of the manufacturers is closely held proprietary information sometimes, but we have an idea of production,” Ryan said, adding. “I think Bavarian Nordic has been very open to discussing how they could scale up production.
“And I do know that GAVI and others are willing to engage around how the existing vaccines beyond donations could also be procured.
“So we are taking the gloves off to join hands in partnership – not to beat anyone around on the head,” Ryan said.
The MVA-BN vaccine as well as a second vaccine, LC16 KMB, produced by the Japanese firm KM Biologics, both present technical challenges in terms of their administration as well, Ryan pointed out. The MVA-BN requires two jabs – a challenge in settings like DRC wracked by conflict and insecurity.
The LC16 vaccine, on the other hand, requires intradermal administration – a relatively simple skin jab, but still a procedure requiring training for the health workers unfamiliar with the technique.
In addition, Ryan added, neither vaccine has yet been formally approved for use in children – and amongst the 250 deaths seen so far in DRC this year, most victims have been children under the age of 15.
Targeting vaccines due to limited supplies
“Given limited supply, limited availability of vaccines need to really be able to use those vaccines in a targeted way to reach those who are most at risk,” Van Kerkhove said.
“We’re currently looking at a number of different ways the vaccines could enter into the country, led by our country office, the Ministry of Health and their partners. We’re looking at bilateral donations, at the use of vaccines as part of a response strategy – at a number of different options apply, but we’re also looking at supply,” she stressed, adding: “We’re looking at how many doses could be available. And then of course the strategies in which those vaccines can be used in outbreak situations.”
Still trying to understand the epidemiology ’
While the barriers remain, virus transmission continues to expand within communities and geographies.
“In 2024 alone there have been more than 3000 suspected cases and about 250 deaths with a crude case fatality ratio around 7.8%,” said Van Kerkhove, of the outbreak, the largest ever seen by the DRC to date.
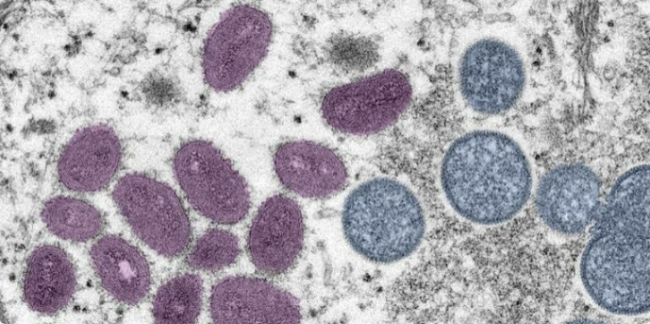
The high fatality rate is due to the fact that most cases seen so far in the DRC have been of the Clade I mpox virus, which very deadly.
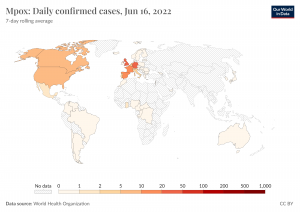
In contrast, it was the much milder Clade II virus that triggered WHO’s declaration of a global health emergency in 2022 – which it began circulating widely outside of Africa, primarily among men who have sex with men. The emergency was declared to be over in 2023, after the successful rollout of millions of vaccines among at-risk groups in high and middle income countries.
As well as being more deadly, the patterns of transmission of the Clade I virus in DRC and West Africa, also appear to be much more varied – although sexual transmission is a factor, it is not the only one.
DRC and global health officials are thus struggling to “better understand the epidemiology,” of the outbreak, which is happening amongs a wide variety of communities and populations – from children to sex workers.
“There are clearly different outbreaks that are happening, some are happening among sex workers, some are zoonotic transmission and some family clusters,” Van Kerkhove said.
“We’re working with our country office in DRC, our regional office and many different partners to look at the types of interventions that can prevent infections, but also stop transmission,” Van Kerkhove said. “And one of those interventions is vaccines.”
“We had a big partnership meeting yesterday. A lot of people are now actively engaged. But let’s be real here. We do have to look at the different types of scenarios and be realistic about how much vaccine is available, how quickly the vaccines can be used, and how they can optimally be used in different parts of DRC and beyond. To have the biggest impact in stopping human-to-human transmission.”
Image Credits: National Foundation for Infectious Diseases , Tessa Davis/Twitter , WHO.
Source: Health Policy Watch